Healthy Weigh Study Results
What strategy works better for weight loss in overweight employees?
- Financial incentives
- Environment change strategies
- A combination of the two,
- On-your-own weight-loss efforts
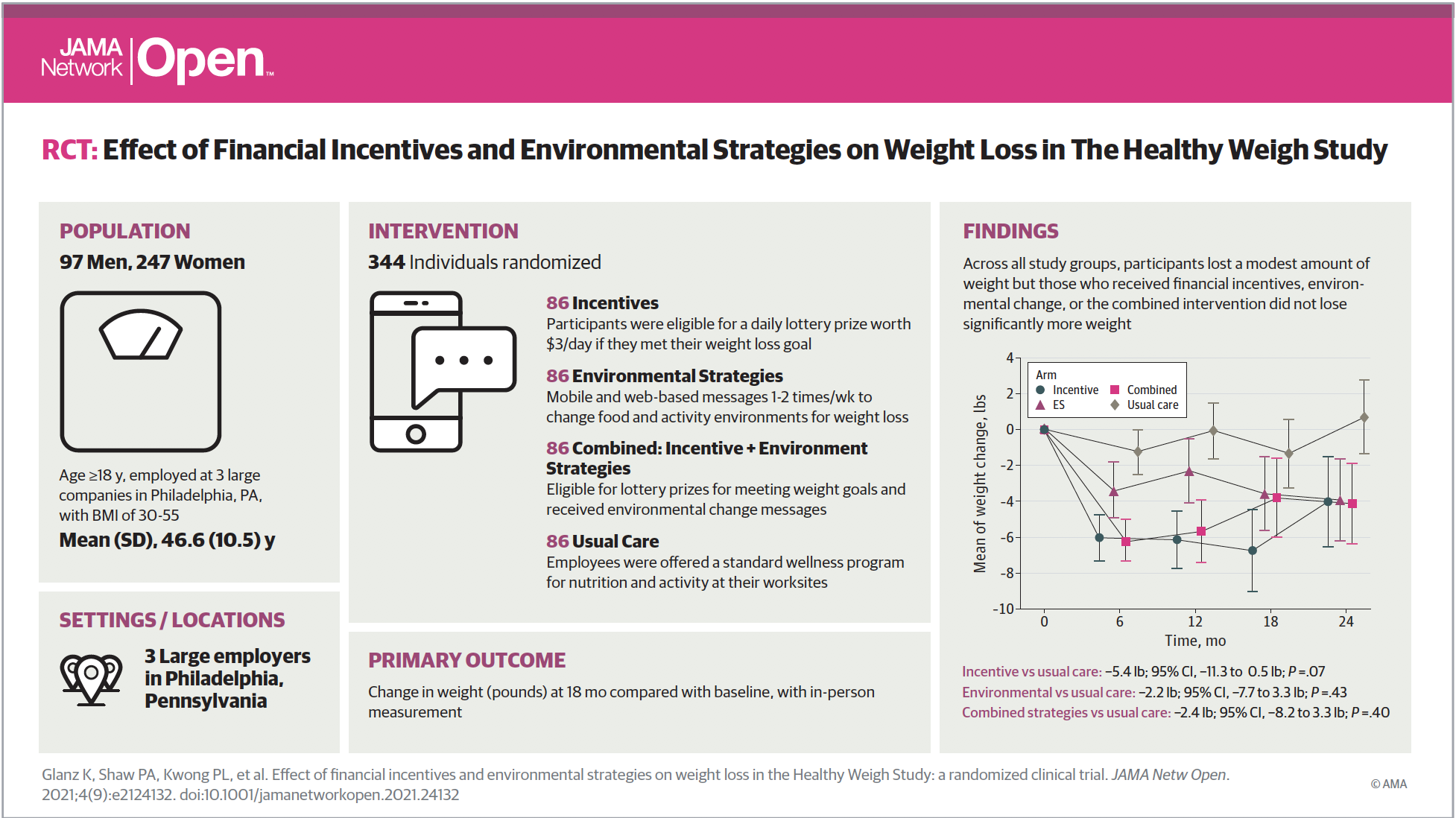
Drs. Karen Glanz and Kevin Volpp, along with the team at the UPenn PRC, found that participants in all groups lost weight. Incidentally, the financial incentives group lost slightly more weight, but none of the strategies netted significantly greater weight losses than the others. The results from their Healthy Weigh Study are currently published in the September 2021 edition of JAMA Network Open.
In 2015, the University of Pennsylvania Prevention Research Center (UPenn PRC) conducted a study to test strategies to achieve weight loss and maintain weight loss in urban worksites in Philadelphia.
First, researchers collected data on participants who earned daily financial rewards, in addition to those guided on positive changes to their environment.
Second, they compared each strategy, separately and together, to see which one helped the participants achieve weight-loss.
Third, the team compared that data to those who tried to lose weight on their own.
Ultimately, the goal of the study was to manage obesity by improving nutrition and physical activity, in order to reduce the risk of cardiovascular disease and other chronic health conditions.
- Read the news brief by Penn Nursing here.
- Find more information about the environmental change strategies in our toolkit, Tips for Losing Weight and Keeping it Off.
- Read the full paper in JAMA Network Open.
Publication
Glanz K, Shaw P, Kwong P, Choi J, Chung A, Zhu J, Huang Q, Hoffer K, Volpp K. Effect of Financial Incentives and Environmental Strategies on Weight Loss in The Healthy Weigh Study: A Randomized Clinical Trial. JAMA Network Open 2021;4(9): e2124132. doi:10.1001/jamanetworkopen.2021.24132

 In the February 16, 2016 issue of Annals of Internal Medicine, UPenn PRC Director Kevin Volpp, MD, PhD, UPenn PRC researcher David Asch, MD, MBA, and co-authors reported on a study to test the effectiveness of offering financial incentives to increase physical activity among overweight and obese adults.
In the February 16, 2016 issue of Annals of Internal Medicine, UPenn PRC Director Kevin Volpp, MD, PhD, UPenn PRC researcher David Asch, MD, MBA, and co-authors reported on a study to test the effectiveness of offering financial incentives to increase physical activity among overweight and obese adults.