Dad left the hospital greatly weakened and spent the next three months in a skilled nursing facility just down the hall from his apartment. I accompanied him on follow-up visits, first with the gastroenterologist. The physician assistant saw him first. When she opened up the medical record on a computer screen, she said, “I see you have pancreatic cancer.” He was taken by surprise, since he thought he was simply having a follow-up visit for the stent placed in his biliary tract. But the cancer was the headline on the medical record — the most important problem that defined him.
Other appointments followed, with the surgeon and oncologist. I asked them for more information about the pancreatic cancer diagnosis. What were his “numbers” or “levels” from the biliary brush cytology? Was there any staging information? As a public health professional teaching in medical and nursing schools, and conducting cancer control research, I wanted more information. I was promised specifics, but never received them, despite my persistence.
Dad’s next visit to the ER occurred a few months later, when he was incoherent after a fall from his bed in the skilled nursing facility. The first reaction by the ER doctors and nurses — he has pancreatic cancer. As it turned out, he had a hip fracture and internal bleeding. He was found to have a healthy enough heart to go ahead with a hip replacement, in the hope that he could walk again.
He never developed any symptoms of pancreatic cancer. There was one more hospitalization, nine months after the first one. He was a very weak 94-year-old and the ER doctors said, “I see he has pancreatic cancer.” This time it was pneumonia and a few days later he entered a residential hospice, where he spent his last five days receiving palliative care from a wonderful hospice team. Cause of death? Sepsis. Other significant conditions contributing to death? Probable pancreatic cancer.
Just a few decades ago, doctors were reluctant to tell a patient about a cancer diagnosis. Now the doctors — really, the records — couldn’t repeat the diagnosis often enough. I was troubled by the possible or probable pancreatic cancer diagnosis and how it dominated his electronic health record. And I was concerned that I never received much information to understand it. So I ordered and paid for his medical records.
It turns out that only the hospital records were provided; I did not receive images of his electronic health record. And it turned out that the pancreatic cancer diagnosis was cut-and-pasted from one record to the next. It was “possible biliary tract cancer or pancreatic cancer” but no definitive diagnosis was made. Apparently, though not written in the record, the imaging tests for further diagnosis were determined to be of little value, and thus were not done.
So was my father his pancreatic cancer? Probably not, and not even the doctors know the whole story. But it seemed like the system failed him, and me and our family. Caregivers are responsible for the accuracy of the records. Cut-and-paste doesn’t cut it. They are also responsible for putting diagnoses in appropriate clinical priority and for being sure that something does not get passed on as a dehumanizing label.
Sooner or later, everyone will become a patient. We need new ways to modify the medical record to preserve its link to the uniqueness of the patient, so the diagnosis doesn’t supersede the person.
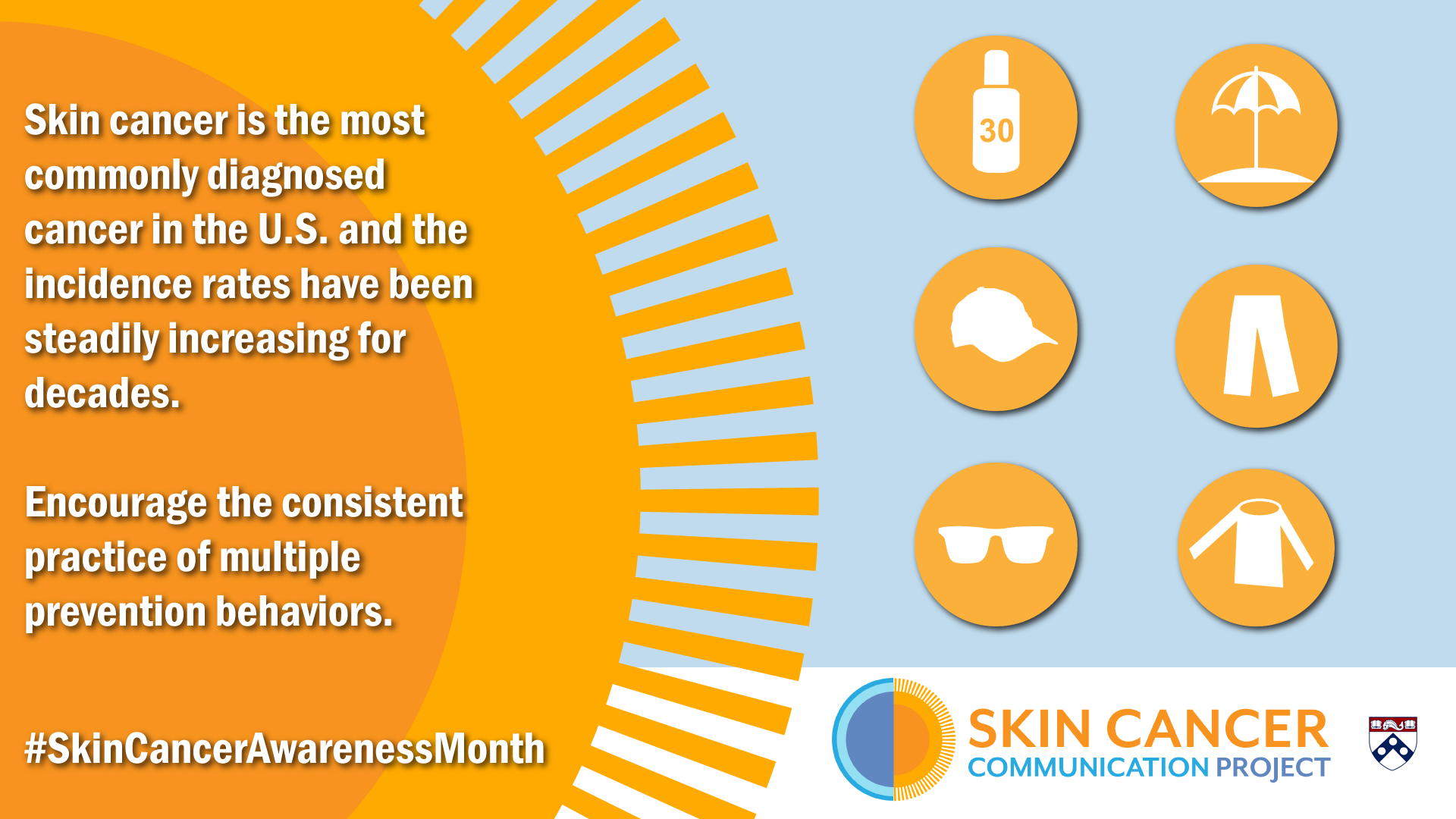
Karen Glanz, PhD, MPH is George A. Weiss university professor of medicine and nursing at the University of Pennsylvania and director of the UPenn PRC.
Op ed via The Philadelphia Inquirer, Viewpoint