Jul 3, 2018
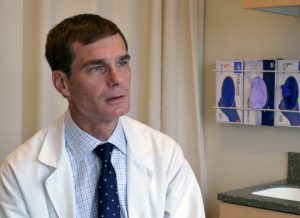
Aging happens differently for everyone and forgetting some details for daily tasks is not always cause for alarm. But there are signs that you or a loved one are showing signs of dementia or other diseases, like Alziemer’s. Dr. Jason Karlawish published an article with AARP as part of their Disrupt Dementia campaign.
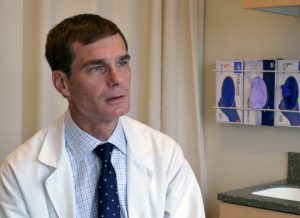 Dr. Karlawish a researcher on the Healthy Brain Research Network and the Cognitive Aging Communication Project, both funded supplements to the UPenn Prevention Research Center. He also serves as the director of the Penn Memory Center. Dr. Karlawish writes about what to look for and the risks involved with allowing the disease to progress without intervention.
Dr. Karlawish a researcher on the Healthy Brain Research Network and the Cognitive Aging Communication Project, both funded supplements to the UPenn Prevention Research Center. He also serves as the director of the Penn Memory Center. Dr. Karlawish writes about what to look for and the risks involved with allowing the disease to progress without intervention.
Read about the signs to look for and his personal experience with an aging parent here. Tweet about your experiences, using the hashtag #DisruptDementia and tag @AARP and @jasonkarlwish.
Jun 18, 2018

A call for Community Scholars
Applications are now being accepted for the Community Scholars-in-Residence program which will be focused on cancer prevention and control research.
Through this program, scholars will develop relationships with a community research partner of their choosing, identify research opportunities, and co-develop research projects during a one to two-year tenure with a community partner organization.
Eligibility: Standing pre/post docs with an interest in conducting community-engaged health research Project Topics: Projects must focus on cancer prevention and control research, and must be co-developed with a community partner Program Duration: 12-24 months Funding: Each Scholar/Community Organization team will receive up to $5,000 for their project Program Start: September 2018. Application Deadline: June 1, 2018 EXTENDED THROUGH JUNE!
Program Structure:
Faculty Mentorship: Scholars will identify a mentor from qualified faculty in the area of cancer prevention and control research. Mentors will guide the development, implementation and evaluation of the project. Scholars are expected to meet with their mentor on a monthly basis. Mentors will receive $500 (for discretionary funds) for their support.
Community Partner Organization: The community partner organization should be identified by the scholar and can include any community organization that provides, plans for, coordinates, organizes, pays for, or regulates health/public health services or impacts health outcomes in the community.
Time Commitment: Scholars will devote an average of 4-6 hours per week to this program and it is expected that a majority of the time will be spent with the community partner.
Formal Training: Scholars will participate in a one-day kick-off workshop that will cover key community-engaged research skills and participate in regular meetings and trainings that will provide opportunities for sharing personal experiences and lessons learned. Representatives from the community partner organizations will be invited to participate in the meetings.
Funding: Scholars will develop a project and submit a proposal for funding (up to $5,000 per project). We suggest building in a minimum of $500 for your host organization.
Please contact Jill McDonald at jillmcd@upenn.edu for more information and a program application.
Funding for this program comes from Community Engagement and Research Core in the Penn CTSA and the UPenn Cancer Prevention and Control Research Network (CPCRN).
Jun 12, 2018
The Student Health Service/Campus Health department at the University of Pennsylvania created videos to accompany their tobacco-free campus campaign. Watch their video, supported by the University of Pennsylvania Prevention Research Center (UPenn PRC), to learn more about their plans to improve health and create a more beautiful and sustainable campus.

Visit their website for more information on this ongoing project and look for the signage that alerts students and staff that Penn is Tobacco Free. Student Health Services has also provided a Tobacco Cessation Resources brochure to help students quit smoking.
May 23, 2018
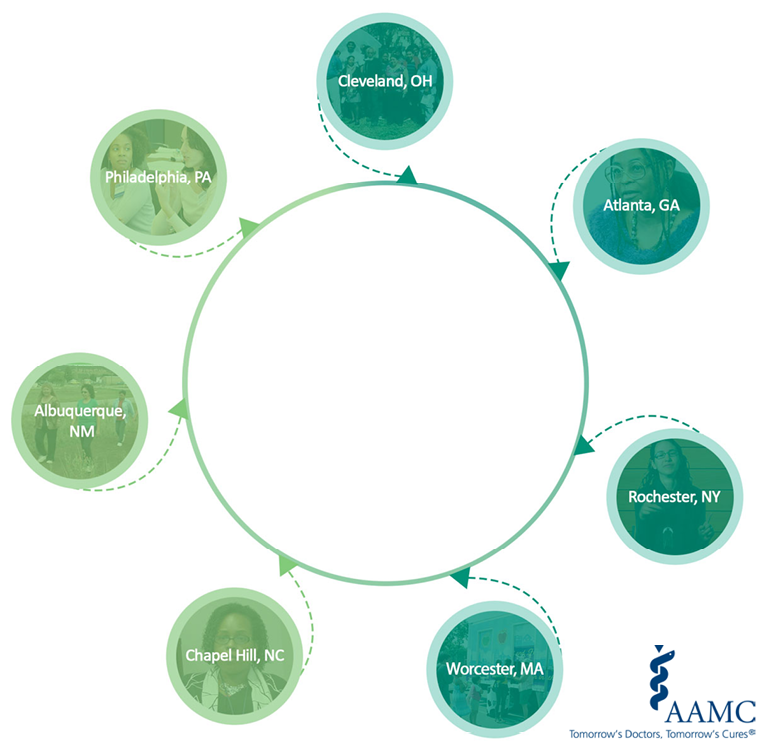
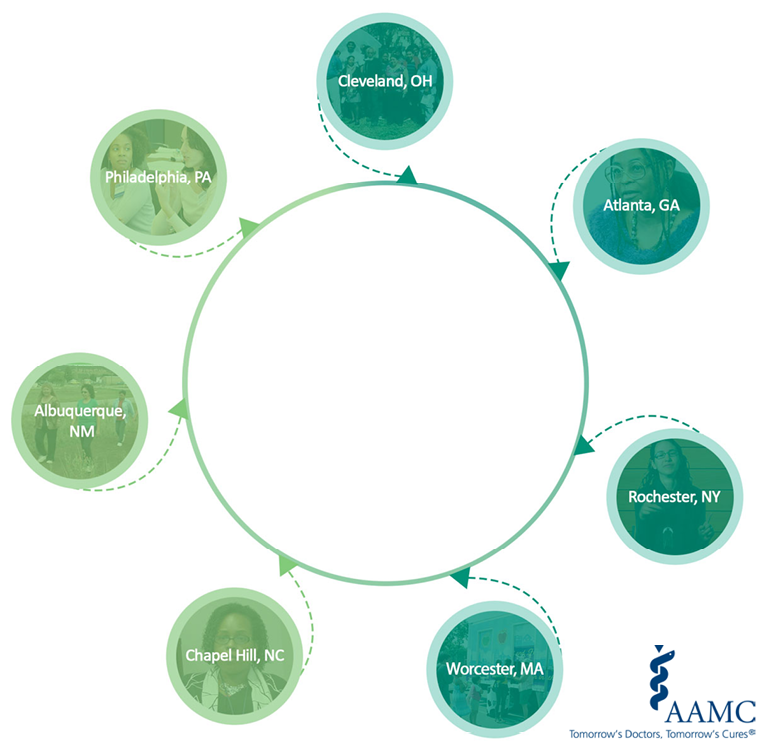
As a part of their continued commitment to improving the health of individuals and populations, academic medical centers are conducting research to find solutions for inequities in health and health care. The 2018 Health Equity Research Snapshot, an initiative of the Association of American Medical Colleges (AAMC), highlights seven videos featuring innovative community-partnered research projects within AAMC member medical schools with preventative medicine residency programs, and explores how people and their communities can avoid or counter risks for chronic illnesses. The effort is a collaboration with the Centers for Disease Control and Prevention’s Prevention Research Centers, a network of 26 academic research centers across the country.
For more information and to view the videos, visit www.aamc.org/healthequitysnapshot.
Click “Philadelphia, PA” to see our video!
May 3, 2018
Stites, S.D., Milne, R., Karlawish, J.
Alzheimer’s and Dementia: Diagnosis, Assessment and Disease Monitoring
Volume 10, 1 January 2018, Pages 285-300
- PRC Investigator, Dr. Jason Karlawish joined S.D. Stites and R. Milne to study how a bio marker-based diagnosis can help a patient during each stage of Alzheimer’s Disease. The stigma or shame that can come with the disease can affect how a patient feels about themselves. Dr. Karlawish and his colleagues explored how changes in the way a patient is diagnosed can help address these stigmas.
Read more about the Healthy Brain Research Network here.
Mar 23, 2018
Indoor tanning is a risk factor for skin cancer, particularly among young, white women. Our researchers found that persuasive health messages that encourage young women to quit indoor tanning should focus on their beliefs that it helps their appearance and mood, rather than the health risks.
20% of our nation’s young, white women indoor tan, knowing the risk of skin cancer. In November and December of 2015, a national online survey was conducted with 279 non-Hispanic white women, ages 18-25 in the United States, who indoor tan.
This survey investigated the young women’s beliefs and attitudes as well as social influences that kept them from quitting.
“Young women were most concerned about skin damage and that quitting tanning might affect their mood,” says Amy Bleakley PhD, MPH, lead author of the study. “It was interesting that quitting tanning to prevent skin cancer did not motivate their intention to quit. Health messages that focus on appearance and mood instead of skin cancer may be more effective in encouraging young women to quit indoor tanning.”
Researchers suggest that health messages from doctors, parents and other loved ones aimed at discouraging indoor tanning should highlight the belief that quitting indoor tanning will reduce skin damage. In addition, messages should counter the belief that quitting will make them less happy. Finally, messages should highlight key people who would approve of them quitting indoor tanning.
Read the article here.
Amy Bleakley, Amy Jordan, Morgan E Ellithorpe, DeAnn Lazovich, Sara Grossman, Karen Glanz
Published: March 15, 2018
Dec 7, 2017
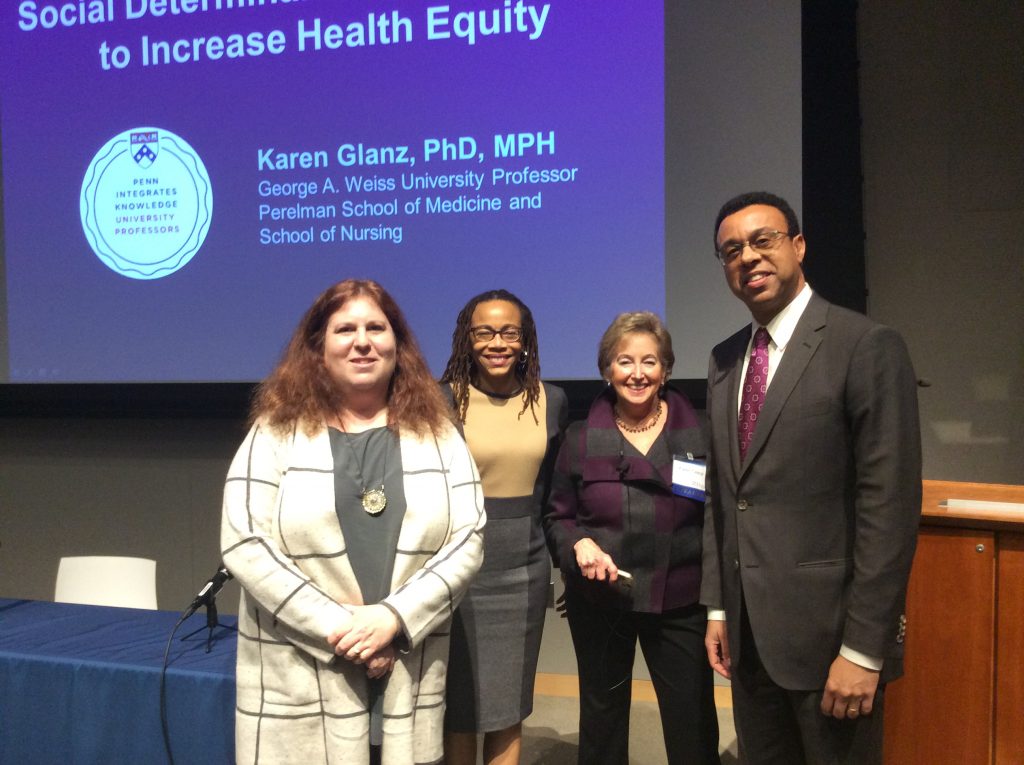
On November 29, 2017, three of University of Pennsylvania’s distinguished professors presented their collaboration on Health Disparities in the second PIK seminar. Penn Integrates Knowledge (PIK) is a program where the hand-picked professors collaborate and “bring knowledge together across disciplines and use that knowledge to illuminate some of the most fundamental issues of our time.”
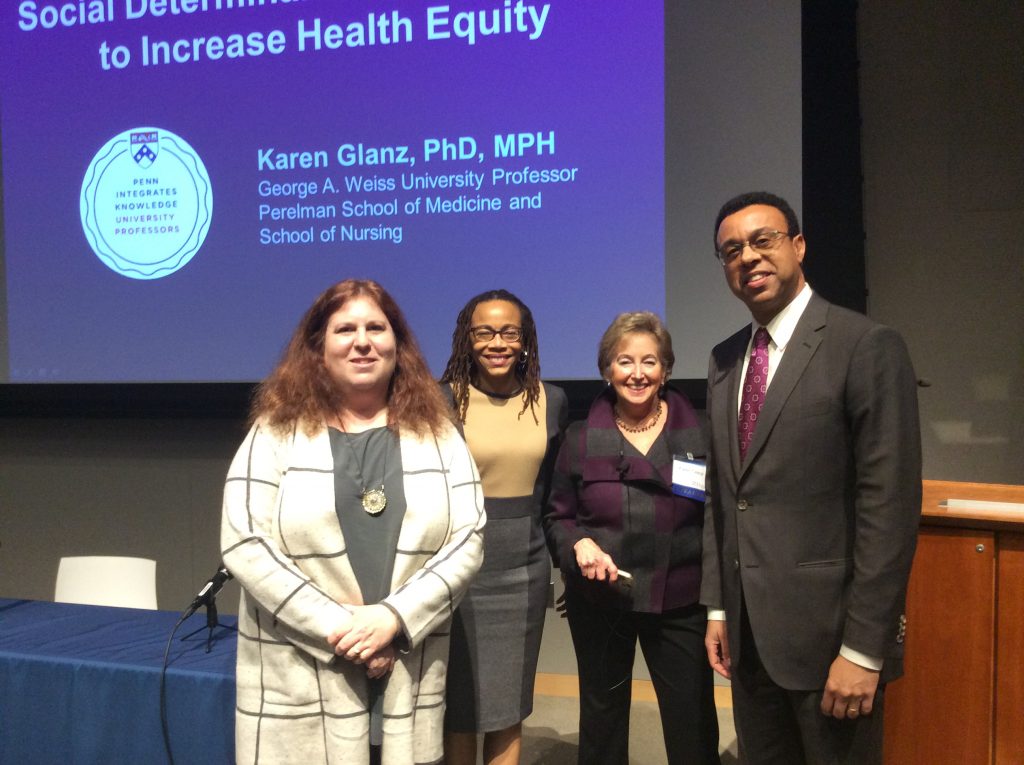
Sarah Tishkoff, Dorothy Roberts, and Karen Glanz with Provost Wendell Pritchett.
The speakers:
- Karen Glanz, MPH, PhD of Perelman School of Medicine and School of Nursing
- Sarah Tishkoff, PhD of the Perelman School of Medicine and the School of Arts and Sciences
- Dorothy Roberts, JD of Penn Law and School of Arts and Sciences
- Introduction by Provost Wendell Pritchett.
They presented their ideas on Health Disparities: Integrating Knowledge from Genomics, Social Sciences and Law to a group of about 140 at the Law Auditorium in the Jordan Medical Education Center. There was a live-stream of the presentation for those that couldn’t make it.
You can view the live-stream video of the seminar HERE.
Each presentation is also featured on the Penn LDI site HERE.
After taking questions, the speakers and audience continued the conversation at a reception in the beautiful atrium.

The atrium at Jordan Medical Education Center.